Translate
Friday, October 30, 2015
Friday, October 9, 2015
Physical activity and Exercise tips for stroke survivors
Stroke is one of the leading causes of long term disability in India. It has emotional, psychological, physical and financial effects on the stroke survivor as well as his/her family. Stroke survivors are predisposed to a sedentary lifestyle that limits performance of activities of daily living, increased risk of falls and heightened risk for recurrent stroke and cardiovascular disease. Activity limitations (also referred to as “disabilities”)
are manifested by reduced ability to perform daily functions,
such as dressing, bathing, or walking. The magnitude of
activity limitation is generally related to but not completely
dependent on the level of body impairment (ie, severity of
stroke). Other factors that influence level of activity limitation include intrinsic motivation and mood, adaptability and
coping skill, cognition and learning ability, severity and type
of preexisting and acquired medical comorbidity, medical
stability, physical endurance levels, effects of acute treatments, and the amount and type of rehabilitation training. All the above effects create a
vicious circle of further decreased activity and greater exercise intolerance, leading to secondary complications such as
reduced cardiorespiratory fitness, muscle atrophy, osteoporosis, and impaired circulation to the lower extremities in stroke
survivors. In addition, a diminished
self-efficacy, greater dependence on others for activities of
daily living, and reduced ability for normal societal interactions can have a profound negative psychological impact
Goals of Physical activity / Exercise
Goals of Physical activity / Exercise
Traditionally, the physical rehabilitation of individuals typically ended within several months after stroke because it was
believed that most if not all recovery of motor function
occurred during this interval. Nevertheless, recent research
studies have shown that aggressive rehabilitation beyond this
time period, including treadmill exercise with or without
body weight support, increases aerobic capacity and sensorimotor function. The three major rehabilitation goals for stroke patients are preventing
complications of prolonged inactivity, decreasing recurrent
stroke and cardiovascular events, and increasing aerobic
fitness.
Preventing complications of prolonged physical inactivity
The stroke patient needs to initiate a physical conditioning regimen designed to regain prestroke levels of activity as soon as possible. For inpatients, simple exposure to orthostatic or gravitational stress (ie, intermittent sitting or standing) during hospital convalescence has been shown to prevent much of the deterioration in exercise tolerance that normally follows a cardiovascular event or intervention. Shortly after hospital discharge, the continuum of exercise therapy may range from remedial gait retraining in hemiparetic stroke patients to supervised or home-based walking or treadmill training programs.
Prevent recurrent Stroke and Cardiovascular events
A reduction of risk factors can decrease the incidence of recurrent strokes and cardiac events. An aerobic conditioning program can enhance glucose regulation and promote decreases in body weight and fat stores, blood pressure (particularly in hypertensive patients), and levels of total blood cholesterol, serum triglycerides, and low-density lipoprotein (LDL) cholesterol. Exercise also increases high-density lipoprotein (HDL) cholesterol and improves cardiac function.
Increasing aerobic fitness
Evidence is accumulating that stroke risk can be reduced with regular leisure-time physical activity in men and women of all ages. It has been proven that men in the moderate- and high-fitness groups had a 63% and 68% lower risk of stroke death, respectively, than men who were in the lowest-fitness group at baseline. Moreover, the inverse association between aerobic fitness and stroke mortality remained even in the presence of cigarette smoking, alcohol consumption, obesity, hypertension, diabetes mellitus, and a family history of heart disease. It is essential that the stroke survivor carries out exercise under the close supervision of qualified medical personnel.
The stroke patient needs to initiate a physical conditioning regimen designed to regain prestroke levels of activity as soon as possible. For inpatients, simple exposure to orthostatic or gravitational stress (ie, intermittent sitting or standing) during hospital convalescence has been shown to prevent much of the deterioration in exercise tolerance that normally follows a cardiovascular event or intervention. Shortly after hospital discharge, the continuum of exercise therapy may range from remedial gait retraining in hemiparetic stroke patients to supervised or home-based walking or treadmill training programs.
Prevent recurrent Stroke and Cardiovascular events
A reduction of risk factors can decrease the incidence of recurrent strokes and cardiac events. An aerobic conditioning program can enhance glucose regulation and promote decreases in body weight and fat stores, blood pressure (particularly in hypertensive patients), and levels of total blood cholesterol, serum triglycerides, and low-density lipoprotein (LDL) cholesterol. Exercise also increases high-density lipoprotein (HDL) cholesterol and improves cardiac function.
Increasing aerobic fitness
Evidence is accumulating that stroke risk can be reduced with regular leisure-time physical activity in men and women of all ages. It has been proven that men in the moderate- and high-fitness groups had a 63% and 68% lower risk of stroke death, respectively, than men who were in the lowest-fitness group at baseline. Moreover, the inverse association between aerobic fitness and stroke mortality remained even in the presence of cigarette smoking, alcohol consumption, obesity, hypertension, diabetes mellitus, and a family history of heart disease. It is essential that the stroke survivor carries out exercise under the close supervision of qualified medical personnel.
Physical Activity and Exercise Recommendations
Stroke survivors:
Benefits of aerobic conditioning:
Preexercise evaluation:
Recommendations for exercise programming:
Stroke survivors:
- Recurrent stroke and cardiovascular disease are the leading causes of mortality in stroke survivors.
- Physical activity remains a cornerstone in the current armamentarium for risk factor management for the prevention and treatment of stroke and cardiovascular disease.
- Activity intolerance is common among stroke survivors, especially the elderly. Their sedentary lifestyle puts them at risk for recurrent stroke and cardiovascular disease.
- Stroke patients achieve significantly lower maximal workloads and heart rate/blood pressure responses than controls during progressive exercise testing.
- Many factors influence activity level after stroke, including physical, mental, and emotional status. Stroke patients may be more disabled by associated cardiac disease than by the stroke itself.
- Energy expenditure during walking in hemiplegic patients varies with degree of altered body structure and function but is generally elevated, often up to 2 times that of able-bodied persons walking at the same submaximal speed.
Benefits of aerobic conditioning:
- Stroke survivors can benefit from counseling on participation in physical activity and exercise training.
- Research studies show that aggressive rehabilitation beyond the usual 6-month period increases aerobic capacity and sensorimotor function.
- An aerobic exercise program can improve multiple cardiovascular risk factors and thereby have important implications for the medical management of stroke survivors.
- Evidence is accumulating that stroke risk can be reduced with regular leisure-time physical activity in multiethnic individuals of all ages and both sexes. Evidence now suggests that the exercise trainability of stroke survivors may be comparable to that of age-matched healthy counterparts.
- Extrapolation of what is known about the training effects of regular exercise by able-bodied individuals suggests that certain levels of exercise that are achieved during many stroke rehabilitation programs may improve aerobic fitness.
Preexercise evaluation:
- It is recommended that all stroke survivors undergo a preexercise evaluation (complete medical history and physical examination, usually including graded exercise testing with ECG monitoring) before they initiate an exercise program.
- When undergoing exercise testing, the testing mode should be selected or adapted to the needs of the stroke survivor (eg, use of handrails, arm cycle ergometry, arm-leg or leg cycle ergometry).
Recommendations for exercise programming:
- Treadmill walking is highly advantageous as the aerobic exercise mode, with inclusion of resistance, flexibility, and neuromuscular training.
- The combination of comorbidities, neurological deficits, and emotional barriers unique to each stroke survivor requires an individual approach to safe exercise programming.
- For patients unable to perform a graded exercise test, light-to-moderate rather than vigorous exercise should be prescribed, with a greater training frequency, duration, or both to compensate for the reduced intensity.
- Subsets of stroke survivors (eg., those with depression, fatigue syndrome, poor family support, or communication, cognitive, and motor deficits) will require further evaluation and subsequent specialization of their rehabilitation program.
- To enhance exercise compliance, the issues of family support and social isolation need to be addressed and resolved.
- Physical activity and exercise training recommendations for stroke survivors should be viewed as one important component of a comprehensive stroke and cardiovascular risk reduction program.
Source: Circulation 2004;109:2031-2041
Saturday, August 29, 2015
Driving after Stroke
Driving after stroke can be a daunting task. It is not only a major concern of individual safety, but, also public safety on the roads. Given the emotional, physical and financial burden of stroke on the stroke survivor's family, it is, but natural for the survivors to want to get back to work as soon as possible. Often survivors don't realize the difficulties that they might have when driving after a stroke. Some may not know all of the effects of their stroke. Driving against doctor's advice is not only dangerous, but also illegal.
How do I know if I can drive?
Many-a-time, the survivors are so keen to get back to normalcy that they ignore some of the signs and symptoms of unsafe driving. After all, they had been doing that for years before the stroke.
Ask your family if they have noticed changes. Those around you may notice changes in your communication, thinking, judgment or behavior that should be evaluated before you drive again. They often have many more opportunities to observe changes than others do.
What are the signs and symptoms of unsafe driving?
How do I know if I can drive?
Many-a-time, the survivors are so keen to get back to normalcy that they ignore some of the signs and symptoms of unsafe driving. After all, they had been doing that for years before the stroke.
Ask your family if they have noticed changes. Those around you may notice changes in your communication, thinking, judgment or behavior that should be evaluated before you drive again. They often have many more opportunities to observe changes than others do.
What are the signs and symptoms of unsafe driving?
- Drives too fast or too slow for road conditions
- Needs help or instructions from passengers
- Doesn’t observe signs or signals
- Makes slow or poor distance decisions
- Gets easily frustrated or confused
- Often gets lost, even in familiar areas
- Has accidents or near misses
- Drifts across lane markings into other lanes
Where can I get help?
Talk to your doctor or occupational therapist. He or she can tell you about your stroke and whether it might change if you can drive. Unfortunately, there are no specific regulations for driving for stroke survivors in India. As such, there are no authorized driver rehabilitation specialists to evaluate driving ability. It would be of great help if the survivors enroll in an authorized driving school and receive instructions on how to modify your driving and the car to compensate for the disabilities. As more capable technologies and new advances in mobility equipment are made each day, wheelchair accessible vehicles have become more powerful than ever before. These modified vehicle solutions – such as hand controls, pedal extensions, seat bases, lifts and ramps – have changed the lives of countless stroke survivors and people with disabilities.
Guidelines in the UK
Driver and Vehicle Licensing Agency (DVLA)/Driver and Vehicle Agency (DVA) sets the rules. After a stroke or TIA you must stop driving immediately, but for many people this is temporary. It is possible to return to driving as long as it is safe to do so and the correct procedures are followed. The DVLA produce a factsheet, Car or motorcycle drivers who have had a stroke or transient ischaemic attack (TIA). This outlines when you have to inform them that you have had a stroke. This guide also applies in Northern Ireland and your medical practitioner may refer to these when advising you.
Cars or motorcycles
If you have a licence to drive a car or motorcycle (category B licence) you are not allowed to drive for at least one month after a stroke or TIA. After a month you may start driving again if your doctor is happy with your recovery. If you have had a number of TIAs over a short period of time you will need to wait until you have not had any TIAs for three months before returning to driving. You will also need to notify the DVLA/DVA.
If you have a licence to drive a large goods vehicle (LGV) or a passenger carrying vehicle (PCV) you must tell the DVLA immediately that you have had a stroke. You are not allowed to drive this type of vehicle for one year. After this time you may be able to resume driving, but this will depend on how well you have recovered and also on the results of medical reports and tests.
Specially adapted cars
Even if you have physical disabilities following your stroke, it may still be possible for you to drive. There are various vehicle adaptations and motoring accessories that can make driving possible and more comfortable. Specialist mobility centres can carry out assessments and provide advice about making adaptations to your vehicle which can enable you to return to driving. They can also provide assessments for passengers who have disabilities, and information on how to safely lift wheelchairs in and out of a car.
Pre-driving assessment tools
1. History to determine previous motor vehicle accidents, number of miles driven, psychosocial aspects, medical conditions and current level of psychological functioning
2. Physical examination to identify subtle physical conditions
4. Off-road driving testing (simulator)
Guidelines in the UK
Driver and Vehicle Licensing Agency (DVLA)/Driver and Vehicle Agency (DVA) sets the rules. After a stroke or TIA you must stop driving immediately, but for many people this is temporary. It is possible to return to driving as long as it is safe to do so and the correct procedures are followed. The DVLA produce a factsheet, Car or motorcycle drivers who have had a stroke or transient ischaemic attack (TIA). This outlines when you have to inform them that you have had a stroke. This guide also applies in Northern Ireland and your medical practitioner may refer to these when advising you.
Cars or motorcycles
If you have a licence to drive a car or motorcycle (category B licence) you are not allowed to drive for at least one month after a stroke or TIA. After a month you may start driving again if your doctor is happy with your recovery. If you have had a number of TIAs over a short period of time you will need to wait until you have not had any TIAs for three months before returning to driving. You will also need to notify the DVLA/DVA.
If you have a licence to drive a large goods vehicle (LGV) or a passenger carrying vehicle (PCV) you must tell the DVLA immediately that you have had a stroke. You are not allowed to drive this type of vehicle for one year. After this time you may be able to resume driving, but this will depend on how well you have recovered and also on the results of medical reports and tests.
Specially adapted cars
Even if you have physical disabilities following your stroke, it may still be possible for you to drive. There are various vehicle adaptations and motoring accessories that can make driving possible and more comfortable. Specialist mobility centres can carry out assessments and provide advice about making adaptations to your vehicle which can enable you to return to driving. They can also provide assessments for passengers who have disabilities, and information on how to safely lift wheelchairs in and out of a car.
Pre-driving assessment tools
1. History to determine previous motor vehicle accidents, number of miles driven, psychosocial aspects, medical conditions and current level of psychological functioning
2. Physical examination to identify subtle physical conditions
- Assess joint mobility of neck, shoulders, wrists, hips, knees and ankles
- Assess upper and lower muscle strength manually
- Assess upper and lower coordination through finger-nose, heel to shin and rapid alternating motion
- Current medication
- Visual fitness
- Mental status
4. Off-road driving testing (simulator)
Monday, August 24, 2015
Impact of red tape on the healthcare in India
India is a great nation of over 1.2 billion people. It stands on a 11,000 year old strong culture that is probably matched only by the Mesopotamian culture. It has survived many invaders such as the Arabs and Europeans. After its independence in 1947, India was faced with many problems - poverty, poor healthcare, illiteracy, population explosion, security threats from neighboring countries, to name a few. Since 1980s, economic reforms have propelled India into a an era of rapid growth and development such that the GDP growth during January–March period of 2015 was at 7.5% compared to China's 7%, making it the fastest growing economy. Despite these developments, healthcare sector lagged behind in responding to the healthcare needs of the nation.
In a recent article in the New England Journal of Medicine, Dr. KS Reddy states "With weak regulatory systems failing to set and enforce quality and cost standards, some patients receive inadequate, inappropriate, or unethical care. 70% of health care expenditures consist of out-of-pocket spending". Today, the private sector accounts for about 80% of outpatient and 60% of inpatient care. The reasons behind this appalling state of affairs are many. Red tape and corruption are among the top causes leading to the current state of affairs. to state an example, the Supreme Court held the government and the Medical Council of India (MCI) guilty for the loss of 3,920 MBBS seats mainly because of lethargic inspection of infrastructure in medical colleges and non-grant of timely permission to colleges to admit students! Red tape swallows all walks of life from education to filling job vacancies to providing healthcare to the people.
Failure on the part of any
hospital to provide timely medical treatment to a person in
need of such treatment results in a violation of the patient's
"Right to Life,” which is guaranteed under Article 21 of the
Constitution of India. This is the closest India has
come to enacting laws similar to The EMTALA (Emergency
Medical Treatment and Labor Act) and the COBRA
(Consolidated Omnibus Budget Reconciliation Act), which
are well recognized in the United States. In 1988, the Honorable Supreme Court of India had stated that every injured person be administered emergency medical care to preserve life and there should be no legal impediment to providing medical care. It is shameful to note that there has been no law to this effect and we, Indians, continue to not care for those in need of emergency medical aid.
How can we change the way we treat our people? Should there be a law enforcing people to care for fellow citizens? Should we punish people who see a person dying but, don't come forward to assist him/her? Should we enforce all the hospitals to provide emergency care? Unfortunately, the problem lies in the mindset of the people more than anything else. How can we get people to care for their fellow citizens? I do not know the answer to this question. But, one thing is sure, IF WE, THE PEOPLE, DO NOT CARE FOR OUR FELLOW CITIZENS, NO ONE ELSE WILL
How can we change the way we treat our people? Should there be a law enforcing people to care for fellow citizens? Should we punish people who see a person dying but, don't come forward to assist him/her? Should we enforce all the hospitals to provide emergency care? Unfortunately, the problem lies in the mindset of the people more than anything else. How can we get people to care for their fellow citizens? I do not know the answer to this question. But, one thing is sure, IF WE, THE PEOPLE, DO NOT CARE FOR OUR FELLOW CITIZENS, NO ONE ELSE WILL
Sunday, August 9, 2015
Monday, June 22, 2015
Friday, June 5, 2015
Do South Asians stand a higher risk of Stroke?
Stroke or Brain Attack is caused by blockage of arteries or veins in the brain or by bleeding in the brain. It is essential for everyone to remember FASTER to be able to identify stroke and seek treatment immediately. The term FASTER stands for
F - Facial droop
A - Arm or Leg weakness
S - Speech disturbance
T - Time - Call 108 immediately
E - Early - Seek immediate treatment
R - Restore blood supply to the brain
Studies have shown that stroke related deaths are higher among people of South Asian descent (India, Pakistan, Sri Lanka and Bangladesh). The prevalence of high blood pressure, diabetes, cardiac disease, smoking, obesity, rheumatic heart disease, infective meningitis and postpartum stroke are higher in these countries than elsewhere. As such, it is no surprise that the incidence of stroke is also higher in these countries. Added to this is the fact that the level of awareness among people is very low.
How can I reduce the risk of stroke?
Find out more about stroke at www.strokesupport.in
F - Facial droop
A - Arm or Leg weakness
S - Speech disturbance
T - Time - Call 108 immediately
E - Early - Seek immediate treatment
R - Restore blood supply to the brain
Studies have shown that stroke related deaths are higher among people of South Asian descent (India, Pakistan, Sri Lanka and Bangladesh). The prevalence of high blood pressure, diabetes, cardiac disease, smoking, obesity, rheumatic heart disease, infective meningitis and postpartum stroke are higher in these countries than elsewhere. As such, it is no surprise that the incidence of stroke is also higher in these countries. Added to this is the fact that the level of awareness among people is very low.
How can I reduce the risk of stroke?
- High blood pressure does not have any symptoms so the only way to check is to have your blood pressure measured regularly. If you are over 40 you should get your blood pressure checked at least once every five years and more often if it is high or you have other health problems. This can be done by your GP, or you can check it yourself with a home testing kit.
- Diabetes is a condition caused by too much sugar (known as glucose) in the blood. Having diabetes almost doubles your risk of stroke. This is because high levels of glucose in the blood can damage your blood vessels, making them harder and narrower and more likely to become blocked. If this happens in a blood vessel leading to or within the brain it could cause a stroke. If you have diabetes, you must have regular check-ups with your GP or at a diabetes clinic to make sure your blood glucose and blood pressure stay at healthy levels.
- Atrial Fibrillation is a type of irregular heartbeat that can cause blood clots to form in the heart. If these clots block the blood supply to your brain, it can lead to a stroke. If you have Atrial Fibrillation you can be treated with blood thinning medication such as warfarin, or drugs called novel oral anticoagulants, which can reduce your risk of stroke by 50–70%
- Cholesterol is a fatty substance and is vital for your body to function properly. Most of the cholesterol in our body is made by the liver, but it can also be absorbed from some of the foods we eat. Too much bad cholesterol in your blood can cause fatty deposits to build up in your arteries and restrict the flow of blood. It also increases the chance of a blood clot developing. High cholesterol has no noticeable symptoms, so you need to have your cholesterol level checked, especially if you are over 40 and have any of the other main risk factors for developing the condition:
- a history of heart disease or high cholesterol in your family
- you are overweight
- you have high blood pressure or diabetes.
- Lifestyle
- Smoking doubles your risk of having a stroke and the more you smoke, the greater your risk. Smoking reduces the amount of good cholesterol in your blood and carbon monoxide from cigarette smoke damages artery walls and makes your blood more likely to clot
- Using gutka, qimam/kimam, paan or naswar is also harmful to your health. Studies have shown that people who use them are more likely to die from a stroke than people who do not. Other products like bidi/beedi and shisha also contain tobacco, so if you smoke these you are at risk of the same kinds of diseases as cigarette smokers, including stroke.
- Regularly drinking large amounts of alcohol greatly increases your risk of stroke.
- South Asian people carry more weight around their waist than the rest of the population. The South Asian Health Foundation suggests that South Asian men whose waist measures over 90cm and South Asian women whose waist measures over 80cm should be considered overweight.
- Eating a healthy, balanced diet can help to lower your blood pressure and the amount of cholesterol in your blood. Eat more fruits, vegetables, fibre and healthy protein and cut down on fat, sugar and salt.
- Steaming, boiling and grilling are all healthier than frying, which adds extra fat. Fried foods such as samosas, pakoras, chips or fried bread like bhaturas or puri should be enjoyed as occasional treats, rather than a regular part of your diet.
- Research shows that regular exercise can reduce your risk of stroke by 27%. You should aim to do at least 30 minutes of moderate physical activity five or more times a week.
Find out more about stroke at www.strokesupport.in
Friday, May 29, 2015
Children and Stroke
It is a myth that stroke occurs only in elderly individuals. Although less common, infants and children can be affected with stroke.
How common are strokes in children?
Stroke occurs in about 1 in every 4000 live births across the world. Population based statistics are not available for India, however, stroke is one of the leading causes of disability and death in children as well. About 50%-80% of children with stroke are left with permanent neurological deficits such as paralysis of arm, leg, cognitive impairment, speech disturbance, etc
What are the causes of stroke in children?
The risk factors for stroke in children are different from those in adults. Common risk factors include
- Heart disease
- Dehydration
- Head and Neck infections
- Trauma
- Moyamoya disease
- Systemic conditions such as inflammatory bowel disease
- Maternal infection in the fluid around the fetus
- Premature rupture of membranes during pregnancy
- Pregnancy related high blood pressure
What are the effects of strokes in children?
- Sudden onset of severe, progressive headache
- Eye movement problems or complete or partial loss of vision
- Sudden numbness or weakness in the face, arm or leg (especially on one side of the body)
- Difficulty speaking or understanding words or simple sentences
- Difficulty swallowing
- Dizziness, loss of balance or lack of coordination
- Loss of emotional control and changes in mood.
- loss of consciousness, seizures
- Sudden inability to move part of the body (paralysis)
- Behavior changes or personality changes, improper language or actions.
Will my child get better?
- Prompt identification, treatment of complications and prevention of another stroke is the cornerstone of treatment of a child with stroke. The clot busting drug tPA is not generally recommended in children as its efficacy has not been studied in this population.
- Recovery from stroke is different with each child.
- In general, most young people will recover more abilities than older people will.
- Children often recover the use of their arms and legs and their ability to speak after a stroke.
List of specialists involved in management of a child with stroke
- Pediatrician - a child health specialist, can often help coordinate multiple issues with child’s general health
- Rehabilitation Specialists - includes doctors such as physiatrists and pediatricians with expertise in child rehabilitation
- Speech Language Therapist - for assessment and help with speech or language challenges
- Neuropsychologist - for assessment and help with learning and education needs
- Psychologist - can assist with the psychological stresses in both child and family that are common in child stroke
- Orthopedic Surgeon - expert in the “mechanical” complications of stroke such as tightness in the arm or leg that might be helped by surgery
- Hematologist - a blood specialist who helps with testing for blood clotting disorders or occasional rare causes of stroke in children
- Neonatologist - a pediatrician expert in newborn care is usually involved early in the care of children diagnosed with acute neonatal strokes
- Neurosurgeon - occasionally involved when certain types of stroke can be helped with surgical procedures
Sunday, May 24, 2015
Friday, May 22, 2015
What is EMRI (Emergency Management and Research Institute)?
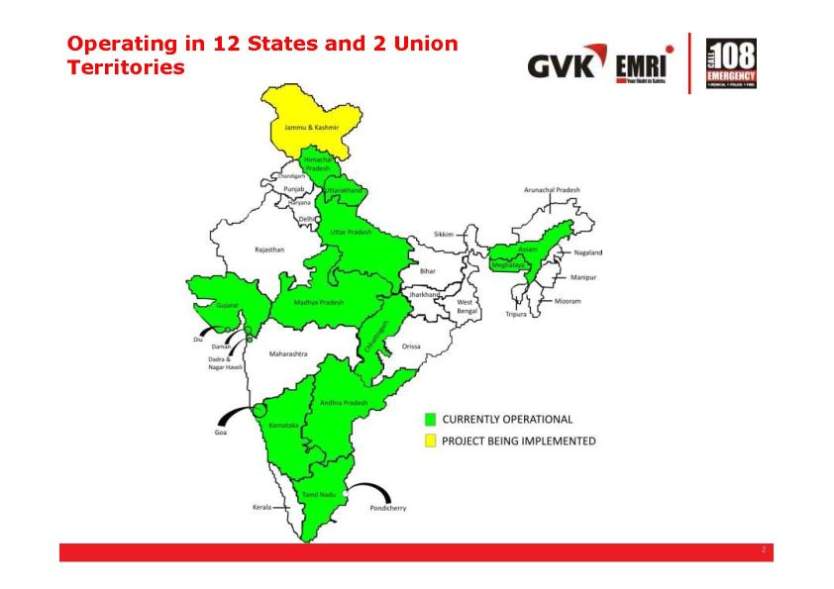
GVK EMRI (Emergency Medical Research Institute) is a non-profit organization providing emergency medical services in India and operating and operating under a Public Private Partnership mode (PPP).
EMRI handles medical, police and fire emergencies through the “1-0-8 Emergency Service". This is a free service delivered through well organized emergency call response centers and staffed by well trained paramedical personnel that are able to dispatch over 2600 ambulances across Andhra Pradesh, Gujarat, Uttarakhand, Himachal Pradesh, Chhattisgarh, Goa, Chennai, Rajasthan, Karnataka, Assam, Meghalaya, Madhya Pradesh, Daman & Diu and Dadra & Nagar Haveli. Beginning in 2005 in Hyderabad, EMRI has become the world's largest integrated Emergency Response Services (ERS) Provider serving 40% of India's population across 12 states and two Union Territories. EMRI has signed memorandums of understanding (MOU) with over 6800 hospitals, which have agreed to provide initial stabilization of EMRI transported patients free of cost for the first 24 hours. In some other states (Rajasthan, Bihar, Punjab, and Trivandrum), Ziqitza has been contracted by the government to operate the 1-0-8 emergency service.
Each ambulance is staffed by a trained EMT (Emergency Medical Technician) who provides pre–hospital care while transporting the patient to a hospital for stabilization. If required, the EMT is able to communicate (via cell phone) with the in house ERCP (Emergency Response Care Physician) who is a qualified medical practitioner, available 24/7 to support the EMT as and when required.
When an emergency is reported through 108, the paramedic, who answers the call, gathers the needed basic information and dispatches appropriate services. Basic information obtained includes:
- Where the call is placed from (district/taluka/city/town/exact location/landmark)
- The type of emergency
- Number of people injured and the condition of the injured
- The caller's name and contact number – for location guidance if required
Emergency help dispatched through this process is expected to reach the site of the emergency in an average of 18 minutes. Pre-hospital care will be given to patients being transported to the nearest hospital.
Ziqitza 108 Emergency Response Service operates in the following states

Friday, May 15, 2015
Apps for Stroke survivors - Apps for Aphasia
Stroke survivors might face difficulties in their day-to-day life because of deficits in speech, memory, etc. There are a number of apple/android apps that are designed to assist stroke survivors in carrying their daily activities and have proven to be very useful. In this post, we discuss some of the common apps that help patients with aphasia (speech difficulty). These apps may be downloaded on iPad/Tablet/Smartphone and help in generating speech, converting text to speech, virtual keyboards, pictures, symbols and video.
Augmentative and Alternative Communication (AAC) is the term used to describe a set of tools and strategies that an individual uses to solve everyday communication challenges. Communication can be in the form of speech, glance, text, gestures, facial expressions, touch, sign language, symbols, pictures, speech-generating devices, etc
Free Apps
Augmentative and Alternative Communication (AAC) is the term used to describe a set of tools and strategies that an individual uses to solve everyday communication challenges. Communication can be in the form of speech, glance, text, gestures, facial expressions, touch, sign language, symbols, pictures, speech-generating devices, etc
Free Apps
- Vox4all® - Android/Apple - is an augmentative and alternative communication (AAC) system for tablets and smartphones. Aims to give voice to those who cannot speak, bridging communication barriers. Using a system of symbols, images, synthesis and voice recording, you can create and configure an environment totally adapted to each user. Available in four languages - English, Spanish, Portuguese, Portuguese.
- Aac Talking Tabs - Android - Uses pictures & symbols-Tap and talk or build phrases. You can create tables or tales and books as well.
- Voice4u - Android/Apple - is an simple application that consists numerous of fun and memorable images that can help assist and improve language. There are over 170 icons consisting of pictures with it’s corresponding word. The icons are included with clear, easy-to-listen audios.
- JABtalk - Android - is a free speech communication application designed to help non-verbal children and adults communicate.
- TapToTalk - Android/Apple - makes communication fun, like another “game” on on an iPad/Tablet. Just tap a picture and TapToTalk speaks. Each picture can lead to another screen of pictures
- SmallTalk - Android/Apple - The SmallTalk™ Family of Communication apps are FREE and offer users extreme portability for practicing speech and communicating on the go
- Dragon Dictation - Android/Apple - Can be used as a therapy device for articulation (feedback on intelligibility) or for people with writing impairment (i.e speech to text)
Paid Apps
- Proloquo2Go ($190) - Apple - It provides natural sounding text-to-speech voices (American, British, and Indian English), high-resolution symbols, automatic conjugations, a default vocabulary of over 7000 items, word prediction, expandability, and accepts your own pictures.
- RocketKeys ($160) - Apple - customizable talking keyboard. This app lets you build the keyboard by choosing the exact keys, size, layout, colors, prediction, and voices you want.
- MyTalk Tools ($49.99) - Android/Apple - helps people with communication difficulties say what they want with sequences of words, sounds and images. You choose the content (simple grids or boards with bold images) and play recorded
- TalkTablet - Android/Apple - for people who have difficulty communicating as a result of autism, aphasia, Down Syndrome, stroke, laryngectomy or any other condition that affects a persons ability to communicate effectively.TalkTablet is the only fully featured AAC speech solution that is compatible with Apple iOS, Android and Kindle handheld and tablet devices.
- Assistive Express ($25) - Apple - is designed to be simple and efficient, allowing users to express their views and thoughts at the most express manner, with natural sounding voices.
There are many more apps available depending upon the need of patients. For a complete list of apps, click on the links below
http://www.stroke.org/sites/default/files/resources/iHOPE-Aphasia-Apps-List.pdf
http://www.stroke.org/stroke-resources/resource-library/aphasia-apps
Saturday, May 9, 2015
Friday, May 8, 2015
Feedback Survey
Dear All,
It has been 7 months since this blog was started with the intention of sensitizing the people and physicians to stroke. To be able to serve the audience better, I would like you all to take this short survey. In addition, we are working on creating a forum to connect stroke survivors and publish their experiences so as to benefit others. A link to the survey is here (it should not take more than 2 minutes to complete the survey):
https://docs.google.com/forms/d/1eJXB3iAU2bYzUIP_yPCfQ_832ISsxQfSIPSKVXGvUMM/edit
Thank you
It has been 7 months since this blog was started with the intention of sensitizing the people and physicians to stroke. To be able to serve the audience better, I would like you all to take this short survey. In addition, we are working on creating a forum to connect stroke survivors and publish their experiences so as to benefit others. A link to the survey is here (it should not take more than 2 minutes to complete the survey):
https://docs.google.com/forms/d/1eJXB3iAU2bYzUIP_yPCfQ_832ISsxQfSIPSKVXGvUMM/edit
Thank you
Saturday, May 2, 2015
Does Air Pollution Affect the Risk of Stroke?
The World Health Organization (WHO) recently published data
on air pollution in various cities across the world focussing on
airborne particles smaller than 2.5 micrometers known as PM2.5. The
report ranked cities after studying their air for the presence of harmful
gases, such as nitrogen dioxide, carbon monoxide and sulphur dioxide, besides
particulate matter (PM) 10 and 2.5. 13 of the world's 20 most polluted cities
are in India, New Delhi being the most polluted of all. Smaller
airborne particles or particulate matter is among the most dangerous of all
these pollutants. New Delhi, Patna, Gwalior, Raipur, Ahmedabad,
Lucknow, Kanpur, Amritsar, Ludhiana, Allahbad, Agra and Khanna are included
among the top 20 most polluted cities in the world.
High levels of air pollution has been linked to increased rate of chronic bronchitis, lung cancer and heart disease. Long term exposure to air pollution has also been associated with higher risk of stroke and impaired cognition. Following are the effects of air pollution on brain and central nervous system:
- Increased risk of carotid atherosclerosis
- Decreased cognition in older people
- Every 2 microgram per meter cube increase in PM 2.5 leads to 1 year of accelerated brain aging and atrophy (degeneration)
- Increased risk of death from stroke among people living in areas with high air pollution, especially in people aged >60 years and non-smokers
- In Tokyo, the risk increase for subarachnoid hemorrhage mortality per 10 μg/m3 PM2.5 or NO2 has been associated with double the risk increase for ischemic or intracerebral hemorrhage mortality
- Stronger associations between short-term air pollution exposure and stroke mortality are observed in elderly, women, and individuals with a history of diabetes mellitus or cardiac disease
- Air pollution on warm days has been more strongly associated with both hemorrhagic and ischemic stroke
/cdn0.vox-cdn.com/uploads/chorus_asset/file/3439174/PM25-QG-Map-Color.0.png)
Friday, April 24, 2015
Intracerebral Hemorrhage
Intracerebral hemorrhage (ICH) is a type of stroke where bleeding occurs within the brain tissue itself. The blood clot causes damage to the brain tissue in that area leading to signs and symptoms. Also, the blood clot may lead to increased pressure in the brain and subsequent symptoms. The bleeding may occur due to a number of reasons such as
- high blood pressure
- head trauma
- arteriovenous malformation rupture
- brain aneurysm rupture
- diseases that cause increased tendency of bleeding (Eg., Hemophilia)
- treatment with blood thinner medicines (Eg., Aspirin, Warfarin, Clopidogrel, Heparin)
- tumors within the brain
- cocaine and amphetamine abuse
- amyloid angiopathy (bleeding due to degeneration of arteries in elderly people)
How common is intracerebral hemorrhage?
About 10% of all strokes occur due to intracerebral hemorrhage while 80% occur due to ischemic stroke (due to blockage of arteries supplying the brain). This translates to about 12-15 cases per 100,000/year in general population. About 40% of patients with intracerebral hemorrhage eventually die and a large proportion of the rest are left with permanent disability. Advancing age and uncontrolled high blood pressure are major risk factors for ICH.
Signs and Symptoms
- Headache
- Nausea and vomiting
- weakness of arm, leg
- facial droop
- confusion, lethargy and loss of consciousness
- speech difficulty
- seizures
- visual loss
- difficulty in walking
How is the diagnosis made?
- A CT scan is the best imaging modality to detect acute bleeding within the brain
- CT angiogram / MRI / MR angiogram and a digital subtraction angiogram may be required to detect the exact cause of bleeding.
How is intracerebral hemorrhage treated?
- The first step in the treatment of intracerebral hemorrhage is to determine the cause of bleed
- High blood pressure is controlled with medications
- If the bleeding leads to increased pressure in the brain, surgery may be needed to remove the clot and relieve the pressure. Surgical procedure may involve craniotomy and evacuation, stereotactic aspiration, draining fluid from the brain.
Recovery and Outcome
Outcome following intracerebral hemorrhage depends upon the cause, location and extent of bleed. Prompt diagnosis and treatment helps to minimize complications and long term sequelae.
Friday, April 17, 2015
Smoking and Brain Aneurysms
The prevalence of brain aneurysms in India is unknown. Extrapolating the estimates in Western countries to India, about 2,00,000 patients suffer from brain aneurysm rupture every year in India. A brain aneurysm rupture is fatal in about 40% of the cases and leads to significant disability in a considerable proportion of survivors. Considering that 62% of India's population is under 60 years of age and that most aneurysm ruptures occur between 35 and 60 years of age, a large proportion of patients lose their productive life due to brain aneurysm rupture.
Smoking is one of the only two modifiable predisposing conditions to brain aneurysm formation and rupture, the other being uncontrolled high blood pressure. According to the data from Global Adult Tobacco Survey (GATS), in 2009-10, about one third of Indians (aged 15 and above) were smokers (48% males and 20% females). As such, every patient with a diagnosed brain aneurysm should be counselled to quit smoking.
Smoking no only predisposes to brain aneurysm rupture, but also acts as a catalyst in aneurysm formation and growth. Some of the known facts about smoking and brain aneurysms are
Smoking is one of the only two modifiable predisposing conditions to brain aneurysm formation and rupture, the other being uncontrolled high blood pressure. According to the data from Global Adult Tobacco Survey (GATS), in 2009-10, about one third of Indians (aged 15 and above) were smokers (48% males and 20% females). As such, every patient with a diagnosed brain aneurysm should be counselled to quit smoking.
Smoking no only predisposes to brain aneurysm rupture, but also acts as a catalyst in aneurysm formation and growth. Some of the known facts about smoking and brain aneurysms are
- Smoking weakens the walls of the arteries in the brain leading to increased risk of outpouching. Also, weak arterial walls promote aneurysm growth and eventually rupture
- Smokers are three times more prone to aneurysm rupture than non-smokers
- Smokers are also predisposed to having stroke more often than non-smokers following aneurysm rupture
- Multiple brain aneurysms (>2 aneurysms) are more common in smokers than in the general population
- Female smokers are at the highest risk of aneurysm rupture
- The phenomenon of vasospasm (narrowing of arteries) following brain aneurysm rupture is more common in smokers
- Smokers are also prone to develop more complications during treatment of the aneurysm (surgical clipping or coiling)
- Even after aneurysm repair by clipping or coiling, the risk of aneurysm re-growth or development of new aneurysms remains in smokers
- High blood pressure and smoking are the only two risk factors for brain aneurysm rupture that can be modified and controlled. Hence, they need to be given utmost importance.
Friday, April 10, 2015
Brain AVMs during pregnancy
An AVM (arteriovenous malformation) of the brain is an abnormal tangle of blood vessels in the brain connecting the arteries to the veins. The tangle of abnormal blood vessels is called a 'nidus'. If the arteries and veins are connected one-to-one without the intervening tangle of blood vessels, it is called a fistula. Because these blood vessels are abnormal, they have a tendency to rupture leading to bleeding within the brain. AVMs are not unique to the brain and can occur in other parts of the body. However, brain AVMs are unique in that they cause severe devastating effects if they rupture.
Brain AVMs diagnosed during pregnancy present a challenge to the neurosurgeon as well as to the obstetrician. The normal changes in the mother during pregnancy may predispose to rupture of the AVM, thus causing brain bleed. If untreated, the AVM runs the risk of bleeding and at the same time, treatment of the AVM may itself pose significant risk to the mother and the fetus. The overall risk of AVM rupture during pregnancy is about 1 in 100,000 deliveries.
What precautions should be taken in a pregnant mother diagnosed with brain AVM
Brain AVMs diagnosed during pregnancy present a challenge to the neurosurgeon as well as to the obstetrician. The normal changes in the mother during pregnancy may predispose to rupture of the AVM, thus causing brain bleed. If untreated, the AVM runs the risk of bleeding and at the same time, treatment of the AVM may itself pose significant risk to the mother and the fetus. The overall risk of AVM rupture during pregnancy is about 1 in 100,000 deliveries.
What precautions should be taken in a pregnant mother diagnosed with brain AVM
- The highest risk of rupture of an AVM is in the second trimester due to the normal pregnancy related changes in the mother.
- The risk of AVM rupture does not increase during labor and delivery and hence, normal delivery should be encouraged
- As the changes occurring in the mother do not immediately revert following delivery, the risk of AVM rupture remains high immediately following delivery
- If the mother presents with seizures, due consideration should be given to the anti-seizure drug as it may harm the fetus
- The symptoms of AVM rupture mimic other common symptoms such as pregnancy induced hypertension and hence a high index of suspicion is required to diagnose a brain AVM
- when a mother presents with severe headache, seizures, speech difficulty or weakness of arm or leg, brain imaging is warranted
- MRI is the preferred method of choice to diagnose brain AVM in pregnancy as it avoids the radiation risk
- Surgery or endovascular therapy for an AVM in a pregnant mother should be carefully thought and undertaken with the understanding all the associated risks such as that of anesthesia, blood loss and radiation. There are no guidelines for the management of brain AVMs during pregnancy
- Stresses associated with normal delivery should be minimized. Primarily, the straining involved in the second stage of labor should be addressed. A combination of an outlet forceps delivery and the use of epidural anesthesia is recommended as means to reduce the duration of labor.
- There is no clear evidence to recommend that women with unruptured AVMs not have children.
- On the other hand, if a woman presents with a history of an AVM rupture in the recent past (within a year), there is evidence to support the recommendation that the patient undergo treatment for the AVM
Friday, April 3, 2015
Brain aneurysms in pregnancy
Pregnancy is a unique phase in a woman's life. It is associated with normal changes in almost every body system that assist fetal survival as well as preparation for labor. High blood pressure (hypertension) is the most common medical problem encountered during pregnancy and complicates 2%-3% of pregnancies. Diagnosis or rupture of a brain aneurysm during pregnancy poses serious life-threatening risk to the mother and the baby. It is therefore imperative that all Obstetricians are aware of this entity so that a high index of suspicion is maintained when pregnant women present with acute headache. The present article discusses some of the common questions about brain aneurysms in pregnancy.
Are brain aneurysms common in pregnancy?
Brain aneurysms rarely present during pregnancy.The reported incidence of brain aneurysm rupture during pregnancy ranges from 3-11 per 100,000 pregnancies. Of all the women presenting with ruptured brain aneurysm during pregnancy, 35% eventually die. It also results in death of the fetus in 17% of the cases. Although brain aneurysms are rare in pregnancy, they account for 5%-12% of all maternal deaths during pregnancy.
Is the risk of brain aneurysm rupture higher in pregnant women than in the general population?
It is unclear whether the risk of aneurysm rupture is higher in pregnant women than in general population. Many studies from Europe have reported increased risk of aneurysm rupture during pregnancy. However, a recent study from the United States reported no evidence of increased risk. The critical periods during pregnancy that can be detrimental to the mother and the fetus are labor and delivery.
How are brain aneurysms managed in pregnant women?
The management of brain aneurysms in pregnant women is similar to that in general population. Additional aspects that should be considered are
Are brain aneurysms common in pregnancy?
Brain aneurysms rarely present during pregnancy.The reported incidence of brain aneurysm rupture during pregnancy ranges from 3-11 per 100,000 pregnancies. Of all the women presenting with ruptured brain aneurysm during pregnancy, 35% eventually die. It also results in death of the fetus in 17% of the cases. Although brain aneurysms are rare in pregnancy, they account for 5%-12% of all maternal deaths during pregnancy.
Is the risk of brain aneurysm rupture higher in pregnant women than in the general population?
It is unclear whether the risk of aneurysm rupture is higher in pregnant women than in general population. Many studies from Europe have reported increased risk of aneurysm rupture during pregnancy. However, a recent study from the United States reported no evidence of increased risk. The critical periods during pregnancy that can be detrimental to the mother and the fetus are labor and delivery.
How are brain aneurysms managed in pregnant women?
The management of brain aneurysms in pregnant women is similar to that in general population. Additional aspects that should be considered are
Asymptomatic unruptured intracranial aneurysm in pregnancy can be managed conservatively with close monitoring with noninvasive imaging techniques such as magnetic resonance imaging. However, expanding or symptomatic unruptured aneurysms in pregnant women should be treated
Radiation exposure to the fetus from CT scan and angiography should be minimized. MRI is the preferred imaging modality. If CT scan and angiography are absolutely required, a lead shield should be used to protect the fetus from radiation.
There are no evidence-based recommendations for child birth in patients with unruptured brain aneurysm, and there is no evidence to suggest that maternal or fetal outcome is improved by cesarean delivery in comparison with closely supervised vaginal delivery. Some studies have recommended caesarean delivery to avoid the stress of labor and delivery.
All women with ruptured brain aneurysms should be treated to prevent rebleeding. Clipping avoids the risk of radiation injury, but puts the mother and the fetus under stress during anesthesia and open surgery. Endovascular coiling poses radiation risk to the fetus.
Friday, March 27, 2015
The importance of support groups in the management of stroke
Stroke, for most people, is a life-changing event in life. Day-to-day activities may seem major obstacles to the stroke survivors. Writing a letter, going to the market, talking to people over telephone and commuting to work may be difficult to perform. Besides affecting the survivor, the family members may also face difficulties ranging from financial burden, strained relationships, frustration, anger and guilt feeling towards the survivor. All these difficulties hinder rehabilitation and recovery of the survivor following stroke.
Support groups allow stroke survivors to help themselves by sharing their experiences with other survivors and learn from others. They also provide a source for emotional and psychological support to survivors who often feel lonely and left out. They also allow the family members and caregivers to share concerns and help each other and bring people together with a sense of common purpose. The survivors and family members often feel empowered because of the warmth, acceptance and emotional support provided by the support group. The stigma associated with disability is eliminated when the survivors connect with other survivors with similar disabilities and this creates a positive attitude to face the problems together. The support groups also help in fundraising to support people in need and further research in the management of stroke.
Some of the popular support groups are
- The American Heart Association (AHA) is one of the oldest, largest voluntary organization devoted to fighting cardiovascular diseases and stroke. Founded in 1924, AHA now includes more than 22.5 million volunteers and supporters working to eliminate these diseases. The AHA also funds innovative research, advocates for stronger public health policies and provide lifesaving tools and information to save and improve lives. The American Stroke Association was created as a division in 1997 to bring together the organization’s stroke-related activities. (http://www.strokeassociation.org/STROKEORG/)
- The United States National Stroke Association provides stroke education and programs to stroke survivors, caregivers, and the healthcare community. (http://www.stroke.org)
- The Aphasia and Stroke Association of India, a nonprofit service organization, is dedicated to increasing public awareness of Aphasia and Stroke. It is committed to promoting the care of individuals with stroke and/or aphasia through educating the public, training families, and assisting with the networking of affected individuals. It is also dedicated to increasing resources that will help improve the quality of life for people with stroke and/or aphasia. (http://www.aphasiastrokeindia.com/index.php)
- The Brain Aneurysm Foundation is a nonprofit organization solely dedicated to providing critical awareness, education, support and research funding to reduce the incidence of brain aneurysm ruptures. (http://www.bafound.org)
- The Aneurysm and AVM Foundation (TAAF) is a nonprofit organization dedicated to bettering the lives, support networks, and medical care of those affected by aneurysm and other vascular malformations of the brain. It is an all-volunteer organization run by survivors, caregivers, and medical professionals. (http://www.taafonline.org)
Friday, March 20, 2015
Rehabilitation after Stroke
Rehabilitation after Stroke is one of the most important phases in recovery after stroke. It is also one of the most neglected aspects of stroke care in India. Annual estimated stroke incidence is 135 to 145 per 100,000, with early death rates ranging from 27% to 41%. This corresponds to ~1.5 million people having a stroke each year, leading to a further 500,000 people, each year, living with stroke-related disability. Hence, every patient being treated for stroke should have access to rehabilitation services.
The long term goal of rehabilitation is to improve function so that the stroke survivor can become as independent as possible. This can be achieved by regaining the lost function as well as retraining other areas of the brain to take up the lost function (brain plasticity).
When does rehabilitation begin?
The long term goal of rehabilitation is to improve function so that the stroke survivor can become as independent as possible. This can be achieved by regaining the lost function as well as retraining other areas of the brain to take up the lost function (brain plasticity).
When does rehabilitation begin?
Rehabilitation should begin as soon as the treating doctor determines that the patient is medically stable. Depending upon the severity of stroke, rehabilitation may be undertaken in
- Rehabilitation unit in the hospital
- At home, through home health personnel
- Outpatient rehabilitation facilities
- Long term care facilities such as nursing home
What are the different components of rehabilitation after stroke?
- Psychological - Depression and anxiety are the most common sequelae after stroke. Timely consultation with a psychiatrist and a psychologist will prevent interference with recovery process.
- Cognitive retraining - The psychiatrist and psychologist can also help in improving communication, spatial awareness, concentration and memory.
- Physiotherapy helps in improving muscle strength and overcoming walking difficulties.
- Occupational therapy involves adapting your home or using equipment to make everyday activities easier, as well as trying to find alternative ways of carrying out tasks that the patients have problems with.
- Speech and Language therapist works with improving difficulties with speech and communication.
- Swallowing difficulty - Some patients may have difficulty swallowing and require a feeding tube to prevent aspiration of food into the lungs. In long term, the speech and language therapist also works with the patient in starting oral feeds in a way to prevent aspiration.
- visual problems such as not being able to see one half of the visual fields may require eye movement exercises and can be addressed by simple ways by the physiotherapist or the ophthalmologist.
- Bladder and bowel problems are not uncommon after stroke and can be effectively be treated with retraining exercises, medications, pelvic floor exercises and the use of special products for incontinence.
- Erectile dysfunction can be a problem after stroke and there are many ways to overcome it.
- Not being able to drive is another major problem that may prevent the stroke survivor from returning to work. It should be borne in mind that the patients should start driving only after obtaining clearance from the doctor. If needed, specific training should be sought.
- Changes should be made in the lifestyle to prevent further strokes.
The ATTEND (Family-Led Rehabilitation After Stroke In India) trial aims to determine whether stroke recovery at home given by a trained family member is an effective, affordable strategy for those with disabling stroke in India when compared to usual care. Considering the cultural and family structure in India, this trial if it is positive it holds promise for a major change in practice in stroke rehabilitation both in developed and developing countries.
Friday, March 13, 2015
Vein of Galen Malformation
Vein of Galen Malformation (VOGM) is a rare condition in which there is an abnormal malformation involving one of the important veins in the brain that returns blood to the heart.
What causes VOGM?
The exact cause of VOGM is unknown. It is seen most often in infants and children. It can be detected as early as during pregnancy during routine ultrasound examination. The condition is not inherited and is not transmitted in the family. Rarely, it can be seen in older individuals.
Signs and Symptoms
The abnormal communication between arteries and veins in the brain leads to increased blood flow into the veins and to the heart. All the symptoms are as a result of this increased blood flow. the most common signs and symptoms are
What causes VOGM?
The exact cause of VOGM is unknown. It is seen most often in infants and children. It can be detected as early as during pregnancy during routine ultrasound examination. The condition is not inherited and is not transmitted in the family. Rarely, it can be seen in older individuals.
Signs and Symptoms
The abnormal communication between arteries and veins in the brain leads to increased blood flow into the veins and to the heart. All the symptoms are as a result of this increased blood flow. the most common signs and symptoms are
- heart failure, often in the first few days of life
- abnormally increased head size and circumference due to excessive fluid accumulation within the brain
- prominent veins on the veins and scalp
- developmental delay
- failure to thrive
- seizures
- headache
- rarely, brain bleed
- if untreated, the condition may be life threatening
Diagnosis
- the condition may be detected on antenatal ultrasound
- CT scan, MRI may be required if there is a suspicion of VOGM
- cerebral angiography is the definitive test to confirm the diagnosis
Treatment
- A Neurosurgeon and neurointerventionist should be consulted to assess the extent and location of VOGM and plan management
- A Cardiologist should be consulted to assess heart function
- The neonatologist or pediatrician takes care of general health of the child
- Embolization is performed to close the abnormal connections. The procedure involves inserting a catheter through one of the arteries in the groin and navigating all the way into the tiny abnormal connections. Coils (metal threads) and glue are used to close the abnormal connections.
- Multiple sessions of embolization are often needed to close all the abnormal connections
- Open surgery for VOGM is never required. However, shunt surgery may be required to drain the fluid from accumulating in the brain.
Outcome
It is often possible to cure the malformation. The extent of brain and heart damage at the time of diagnosis and treatment determines the outcome.
Support Group
VOGM Patents' Alliance http://vogmparents.org/
Friday, March 6, 2015
The Road to Recovery after Brain Aneurysm Treatment - Emotional Effects
"I know all about time and wounds healing, but even if I had all the time in the world, I still don’t know what to do with all this hurt right now.”
------------― Nina Guilbeau, Too Many Sisters
It is impossible for others to understand the suffering that a patient with an illness goes through simply because the experience is unique to the person. The life-changing experience that one goes through after brain aneurysm treatment puts the patient through great emotional stress. Even though no one may truly understand the emotional effects following brain aneurysm treatment, all patients should know that help and support is available. Maintaining a positive attitude, healthy diet and following doctor's advice will help the patient overcome the emotional sequelae.
Common emotional disturbances following brain aneurysm treatment are
------------― Nina Guilbeau, Too Many Sisters
It is impossible for others to understand the suffering that a patient with an illness goes through simply because the experience is unique to the person. The life-changing experience that one goes through after brain aneurysm treatment puts the patient through great emotional stress. Even though no one may truly understand the emotional effects following brain aneurysm treatment, all patients should know that help and support is available. Maintaining a positive attitude, healthy diet and following doctor's advice will help the patient overcome the emotional sequelae.
Common emotional disturbances following brain aneurysm treatment are
Depression: Many brain aneurysm survivors suffer from depression. Symptoms include mood swings, feeling of sadness, anxiety, emptiness, hopelessness, decreased energy and fatigue, difficulty concentrating, forgetfulness, lack of sleep, decreased appetite, loss of interest in pleasure or activities including sex and suicidal thoughts.
The patients need to openly share their feelings with someone close to them and also to the treating doctor. Consultation with a psychiatrist or a psychologist may help. The patients should understand that patience and time are required to overcome some of these sequelae. The most important thing that the patients and their families should understand and keep in mind that having a brain aneurysm is not the end of the road and that help is available to face the emotional and physical disturbances.
Loss of Emotional Control: Many patients experience increased anger, sadness or apathy. The anger or frustration of not being able to go back to the pretreatment state can be difficult to understand. In these circumstances, counselling should be sought.
Loneliness: Many patients feel lonely as they do not have someone to share their suffering. In such circumstances, sharing their feelings with the doctor and seeking appropriate counselling often helps.
Sleep Disturbances: Many patients experience decreased or excessive sleep due to prolonged stay in the hospital or the ICU. In most circumstances, the treating doctor is able to help.
Decreased Self-esteem: Many patients feel less capable of doing their work. In many patients, it is the lack of right attitude rather than physical incapability. Appropriate and timely treatment by a psychiatrist or a psychologist is very helpful.
Family and financial issues: Disputes in the family or financial insecurity may crop up and play a major role in worsening the above mentioned emotional effects. The patient and his/her family should understand that having a brain aneurysm is not the end of the road and, with appropriate and timely treatment, the physical and emotional effects can be minimized.
Friday, February 27, 2015
The Road to Recovery after Brain Aneurysm Treatment - Physical Effects
Having a brain aneurysm and undergoing treatment is a life changing event. Recovery is more difficult and longer in older patients, following brain aneurysm rupture and chronic medical problems. Patients recovering after treatment of brain aneurysm often have physical, emotional and psychological issues. Besides the patient, the family also suffers from many issues, one of the most important being financial burden in Indian scenario. In the coming few posts, I will discuss the issues faced by patients and family and how to get over them
Neurological
Neurological
- weakness of arm, leg
- speech problems
- memory problems
- visual problems
- loss of smell or taste
- difficulty walking or balance problems
- seizures
- fatigue and generalized weakness
- sleep problems
- back pain
Many of these problems gradually improve over time. Evaluation by a physiotherapist and occupational therapist is recommended in patients with arm or leg weakness and balance problems. Speech therapy can help many patients with difficulty understanding and speaking. Appropriate neuropsychological testing and therapy can help patients with memory and behavioral problems to cope with the frustration. Some of the common memory problems include absorbing, storing and recalling information. The memory problem may be from the bleed or stroke during the acute period after aneurysm rupture. Organizing one's daily activities and writing down information is helpful.
Patients with visual problems and seizures should be careful not to drive and should avoid working near heavy machines that can cause injury. evaluation by an ophthalmologist is advised for visual rehabilitation.
Fatigue and generalized weakness is a common complaint in many patients. The patients should understand that it is normal to be sleepy and not interested in outdoor activities for a few weeks. The bleeding in the brain takes a few weeks to resolve. Eat well and engage your mind in activities to keep you busy. Trouble sleeping in the night is also very common and should get better with time.
Back pain may occur in some patients due to lying in the bed for many days or if the bleeding extended into the spine. The headache may also be from spinal tap in some patients. The pain usually resolves in a few weeks as the patients involve themselves in activities.
Common problems following surgery for brain aneurysms are
- incision site pain and numbness - may patients complain of local pain at the site of incision in the scalp following surgery. Some may have numbness over the incision site. The pain and numbness usually goes away with time.
- jaw pain - many patients may have jaw pain on the side of surgery, especially while eating or chewing hard food. For this reason, it is advisable to eat soft food immediately after the surgery. The jaw pain occurs due to manipulation of muscles during surgery and resolves slowly after surgery in about a month.
- clicking sound in the head - some patients may notice a click in the head following surgery. It is also a normal phenomenon and usually resolves in a few weeks
- headache - some patients may have intermittent mild headache that disturbs their daily activity. The pain usually resolves with pain pills or by itself. If headache is severe, associated with vomiting or blurring of vision, consult your doctor immediately.
Common problems following coiling or stenting for brain aneurysms are
- groin pain - there may be bruising or pain in the groin for a few days after the procedure. Please consult your doctor immediately if there is sudden bleeding from the puncture site or painful swelling.
- hair loss - is seen in some patients secondary to radiation. It is more common when the procedures last longer than about 3 hours. The hair loss is temporary in most of the patients.
- headache - may occur in some patients and is usually due to the bleed that occurred following aneurysm rupture. it resolves gradually on its own.
- general bruises over the body - may occur in some patients who take blood thinner pills following stenting. Try not to get hurt or cut yourself inadvertently. If you notice a bad bruise, contact your doctor immediately.
Subscribe to:
Posts (Atom)



